Leadership Message
In my experience, no patient wants to go to the emergency room. There is usually a lot of waiting and it is costly: ED visits cost 12 times more than an office visit and 10 times more than an urgent care visit1. Additionally, studies suggest that as many as 60% of ED visits are patients with at least one chronic condition, and a large number of these visits are preventable with high-quality primary care. Patients with chronic health conditions need access to proactive and well-coordinated primary care teams to ensure that their conditions are well managed2. We all know that keeping patients out of the ED means we sometimes work that patient in to a busy schedule, but more often it involves teams managing chronic health conditions well. At C3, we are thinking about ways to help our practices achieve the goal of reducing these visits over time.
Care Management
Care managers have expertise in identifying root causes for high ED utilization, connecting patients with community resources, helping to set goals and action plans, and supporting behavior change. This makes them uniquely suited to help patients avoid the ED unnecessarily.
RN care managers often reach out to patients after they have been to the ED and educate them as to how they might avoid the ED in the future, if appropriate. Additionally, RN care managers partner with primary care providers to support high-risk patients in between office visits.
Social determinants of health or “economic and social conditions that influence the health of people and communities”1-3 are cited as one of the largest contributing factors to avoidable ED utilization. Patient behavior and social conditions are complex and many patients benefit from an RN care manager who helps them on an ongoing basis.
Mr. Sanders* is a 61-year-old male with progressive Parkinson’s disease. He was living independently when C3 was contacted about his case.
C3 was contacted after Mr. Sanders made multiple visits to the emergency department. In one month, he had been seen a total of 11 times in the ED, with three of those visits resulting in hospital admission. Our RN care manager outreached Mr. Sanders and learned he was struggling to manage his Parkinson’s disease while living independently. The RN care manager also learned Mr. Sanders was having problems taking his medications correctly, and that his medical condition was declining. He did not have family members or friends to assist him with medications. He was very reluctant to transition to an assisted living arrangement, but recognized his struggle to manage his disease.
After further conversations, Mr. Sanders agreed to consider assisted living. The RN care manager worked with the patient, his insurance case manager, the hospital care management team, and his primary care provider to find an appropriate assisted living facility for him. After making the move, his visits to the ED decreased, and he was able to get to his regular PCP and specialist appointments.
*Patient name has been changed.
If you would like more information about how our RN care managers can support patients with high ED utilization, please contact Jennifer Countryman.
1What are social determinants of health? CDC. Accessed August 13, 2022. https://www.cdc.gov/nchhstp/socialdeterminants/faq.html#what-are-social-determinants
2Agency for Health Care and Quality. Accessed on August 31, 2022.
https://www.hcup-us.ahrq.gov/reports/statbriefs/sb268-ED-Costs-2017.jsp
3UnitedHealth: Healthcare could save $32B Annually by Diverting Avoidable ED Visits. Accessed on August 31, 2022. https://www.fiercehealthcare.com/payer/two-thirds-ed-visits-avoidable
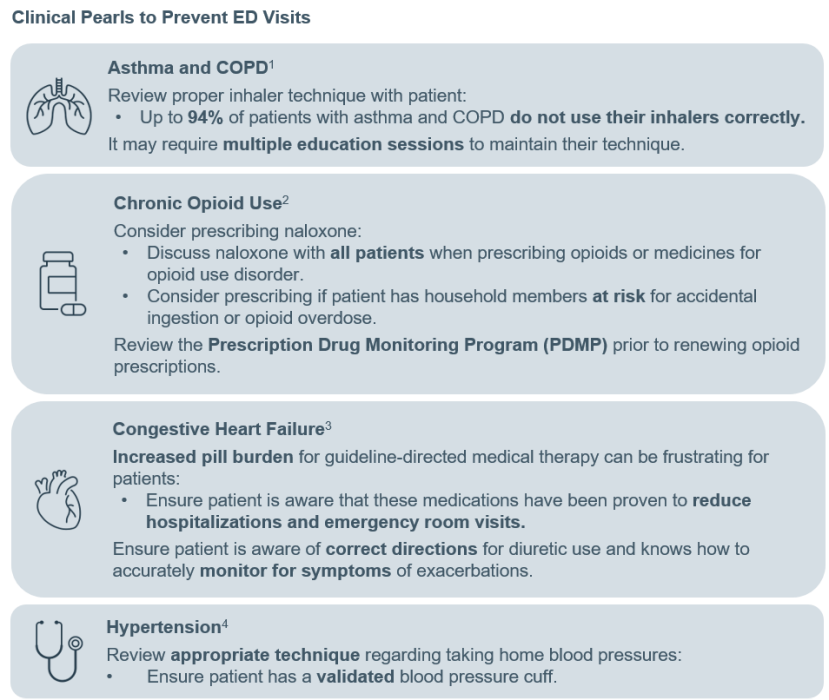
Pharmacy
Patients’ knowledge of their disease states and proper use of their medications—including adherence or non-adherence—play a large role in preventable ED visits. Our pharmacy team has put together some questions to consider when assessing patient understanding, and some clinical pearls regarding disease-specific medication use that can help identify opportunities for education, additional support and optimization of medication therapy.
Assessing patient understanding of chronic diseases and medications.
- Do you understand your disease state and the steps to take to keep you healthy and out of the hospital?
- Are your medications affordable?
- Do you feel your medications are working? Are you having side effects to your medications?
- How do you take your medications or use your inhalers?
- How many doses of your medications do you miss per week?
- How do you check your blood pressure? When do you check your blood sugars? How often do you monitor your weight?
References:
1. Jahedi L, Downie S, Saini B, Chan H, Bosnic-Anticevich S. Inhaler Technique in Asthma: How Does it Relate to Patients’ Preferences and Attitudes Toward Their Inhalers? J Aerosol Med Pulm Drug Deliv. 2017;30(1):42-52.
2. New Recommendations for Naloxone. Content last reviewed August 2020. U.S. Food and Drug Administration. https://www.fda.gov/drugs/drug-safety-and-availability/new-recommendations-naloxone
3. Heidenreich P, Biykem B, Aguilar D, et al. 2022 AHA/ACC/HFSA Guideline for the Management of Heart Failure: A Report of the American College of Cardiology/American Heart Association Joint Committee on Clinical Practice Guidelines. 2022;145(80):e895-e1032.
4. 2017 ACC/AHA/AAPA/ABC/ACPM/AGS/APhA/ASH/ASPC/NMA/PCNA Guideline for the Prevention, Detection, Evaluation, and Management of High Blood Pressure in Adults: A Report of the American College of Cardiology/American Heart Association Task Force on Clinical Practice Guidelines. J Am Coll Cardiol. 2018;71:e127-e248.
Risk Coding
While risk coding may not play an obvious role in preventing ED visits, accurate coding and thorough documentation ensures that patients with chronic medical and behavioral health conditions are identified and have access to payer-supported resources to help manage those conditions.
Here are some diagnosis codes that, when appropriately coded to the higher specificity, help to identify those patients who may require complex patient care management:
- Diabetes with hyperglycemia (E11.65) versus Diabetes, uncomplicated (E11.9)
- Chronic kidney disease stage 5 (N18.5) versus Chronic kidney disease (unspecified)
- Opioid dependence (F11.20) and Chronic pain syndrome (G89.4) versus Low back pain (M54.5)
- COPD (J44.9) versus Moderate persistent asthma, uncomplicated (J45.0)
- Major depressive disorder, recurrent, moderate (F33.1) versus Depression (F32.A)
Select the diagnosis code that provides the most information about the patient’s condition.
- Instead of Anxiety (F41.9), select a further specified diagnosis that discusses the root of the patient’s condition:
– Bipolar disorder, current episode, mixed, mild (F31.61)
– Bipolar II disorder (F31.81)
– Borderline personality disorder (F60.3)
– Other specific personality disorder (F60.89)
– Other childhood emotional disorders (F93.8) - Instead of Headache, unspecified (R51.9), select a further specified diagnosis that clarifies the nature of the headache:
– Migraine, unspecified, not intractable, without status migrainosus (G43.909)
– Periodic headache syndromes in child or adult, not intractable (G43.C0)
Using these codes places your patients in the proper “bucket” and/or outreach call list to make sure that these patients are being seen by their primary care providers and having their chronic conditions managed in a more efficient and cost-effective venue.
Performance
In 2021, our network saw a distinct rise in ED utilization, up from pandemic lows in 2020. This was consistent with national trends, and expected as patients started coming back for care. We are encouraged, however, to see that this rising trend has leveled off in the first quarter of 2022. Additionally, in 2021, our network’s ED/1,000 rates trended the same or better than market rates for Anthem Commercial, Cigna Commercial and Anthem MA patients. While we still have work to do to be the best in every C3 contract, we are making great progress. Great work, teams!
One more VERY EXCITING ANNOUNCEMENT:
In our 2021 commercial contracts, C3 earned shared savings in both Anthem Commercial and Cigna Commercial. These funds were distributed to network practices at the end of August in accordance with C3’s “single funds flow,” which considers member months, payer-reported risk scores and Single Scorecard performance.
Analysis of our performance revealed that in 2021, we kept our medical costs below target; we continued to invest in infrastructure to support our care teams; and we did well in quality. Additionally, we had a higher risk score than the market, reflecting patients with a higher disease burden and providing financial resources to care for these patients. All of these factors helped create the shared savings for our network practices.
Congratulations to everyone on achieving such great results in our commercial value-based programs in 2021—and thank you for your contributions to this success!
Announcements
New Contracts for 2023:
- Aetna Commercial
- Humana Medicare Advantage
- Medicare Shared Savings Program (MSSP) via Caravan Health
New Recorded Educational Opportunities
We continue to add new recorded educational opportunities to our website. Please check back regularly to see what’s new. Providers who view these videos and complete the corresponding survey receive Single Scorecard credit and also have the opportunity to apply for CME credit(s).
New topics in 2022:
- Adolescent Mental Health Town Hall
- Diabetes (coming soon)
- Improving Risk Scores Through Coding and Documentation Town Hall
- Pharmacy and Value-based Care Town Hall
- Risk Coding Series: Pediatrics, Persistent Conditions, Suspect Conditions and Missing Conditions (coming soon)
- Team-based Care and the AWV Town Hall
- 2022 Single Scorecard